What is breast biopsy? (biopsy needle bracket for linear array transducer)
A breast biopsy is a test that removes tissue or sometimes fluid from the suspicious area. The removed cells are examined under a microscope and further tested to check for the presence of breast cancer. A biopsy is the only diagnostic procedure that can definitely determine if the suspicious area is cancerous.

The good news is that 80% of women who have a breast biopsy do not have breast cancer.
There are three types of biopsies:
- Fine-needle aspiration
- Core-needle biopsy
- Surgical biopsy
The latter two are the most commonly used on the breast.
There are several factors that help a doctor decide which type of biopsy to recommend. These include the appearance, size, and location of the suspicious area on the breast. Before discussing biopsy results, let’s first distinguish between the three types of biopsies.
What is fine-needle aspiration?
In most cases, a fine needle aspiration is chosen when the lump is likely to be filled with fluid. If the lump is easily accessible or if the doctor suspects that it may be a fluid-filled cystic lump, the doctor may choose to conduct a fine-needle aspiration (FNA). During this procedure, the lump should collapse once the fluid inside has been drawn and discarded. Sometimes, an ultrasound is used to help your doctor guide the needle to the exact site, whereby sound waves create a picture of the inside of the breast.
If the lump persists, the surgeon or radiologist, a doctor who specializes in medical imaging such as x-rays and mammograms, will perform a fine needle aspiration biopsy (FNABx), a similar procedure using the needle to obtain cells from the lump for examination.
What is a core-needle biopsy?
Core needle biopsy is the procedure to remove a small amount of suspicious tissue from the breast with a larger “core” (meaning “hollow”) needle. It is usually performed while the patient is under local anesthesia, meaning the breast is numbed. During the procedure, the doctor may insert a very small marker inside the breast to mark the location of the biopsy. If surgery is later required, the marker makes it easier for the surgeon to locate the abnormal area. Even if no further treatment such as surgery is needed, the marker allows a breast imaging radiologist to see on future mammograms where the biopsy was done.
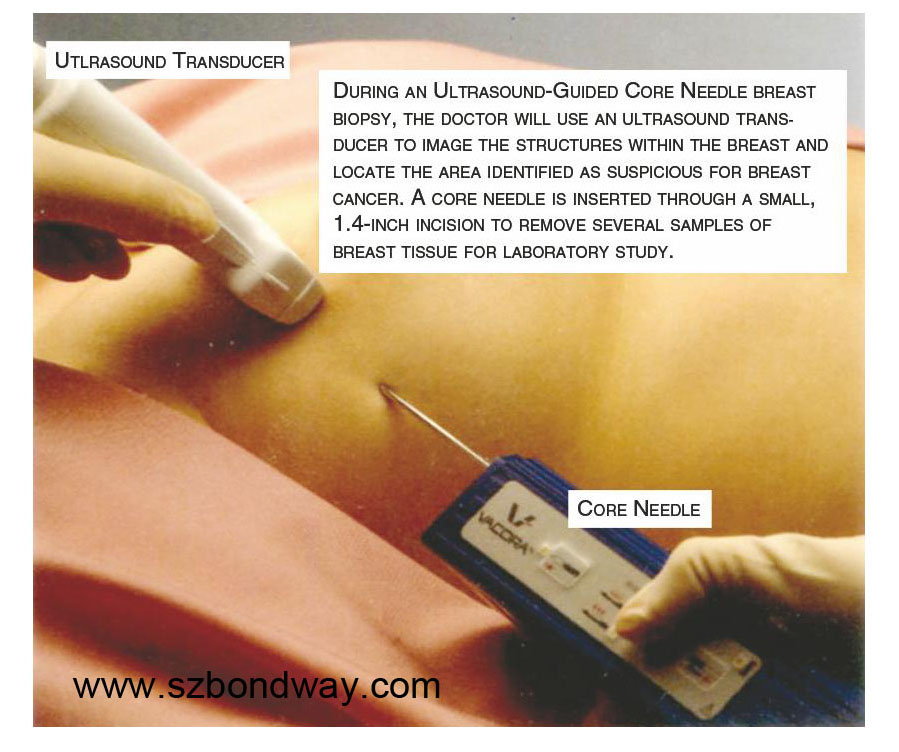
The radiologist or surgeon performing the core-needle biopsy may use specialized imaging equipment to guide the needle to the desired site. As with fine-needle aspiration, this may involve ultrasound.
During an ultrasound-guided core needle biopsy, the patient lies down while the doctor holds the ultrasound against the breast to direct the needle. On the other hand, during a stereotactic-guided core-needle biopsy, the doctor uses x-ray equipment and a computer to guide the needle. Typically, the patient is positioned lying on the stomach on a special table that has an opening for the breast, and the breast is compressed, similar to a mammogram.
Occasionally, no imaging equipment is used, but this is typically only in cases where the lump can be felt through the skin. This type of procedure is called a freehand core-needle biopsy.
There are fewer side effects associated with a core-needle biopsy than with surgical biopsy.
What should I expect from a surgical biopsy?
(Also known as “wide local excision,” “wide local surgical biopsy,” “open biopsy,” or “lumpectomy”)
As with a core-needle biopsy, a surgical biopsy is done while the patient is under local anesthesia. Typically, this test is performed in a hospital setting where an IV and medications are administered to make the patient drowsy.
The surgeon makes a one- to two-inch cut on the breast and then removes all or part of the abnormal lump and often a small amount of normal-looking tissue, known as the “margin.” If the lump cannot be easily felt but can be seen on a mammogram or ultrasound, a radiologist may insert a thin wire to mark the suspicious spot prior to the surgeon performing the biopsy. Once again, a marker is usually placed internally at the biopsy site at the conclusion of the procedure.
What Can Be Learned From The Biopsy Results?
Once the biopsy is complete, a specially trained doctor called a pathologist examines the tissue or fluid samples under a microscope, looking for abnormal or cancerous cells. The pathology report, which can take one or two weeks to complete, is sent to the patient’s doctor. It indicates whether the suspicious area is cancerous and provides a full picture of your situation. For the patient, waiting for results can be a real challenge, but being able to make an informed decision regarding your treatment is well worth it. Your doctor will go over the report with you and, if necessary, discuss the treatment options.
If no cancer cells are found, the report will indicate that the cells in the lump are benign, meaning non-cancerous. However, some type of follow-up or treatment may still be needed, as recommended by the healthcare professional.
If cancer cells are found, the report will provide more information to help determine the next steps.
The report for a core-needle biopsy sample will include tumor type and the tumor’s growth rate or grade. If cancer is found, the pathologist will also perform lab tests to look at cells for estrogen or progesterone receptors.
In the case of a surgical biopsy, the results reveal data about the type, grade, and receptor status of the tumor, as well as the distance between the surrounding normal tissue and the excised tumor. The margin, as we mentioned earlier, shows whether the site is clear of cancer cells.
A positive margin means cancer cells are present at the margin of the tumor. In cases of positive margins, the cancer has spread beyond the immediate area.
A negative margin or clear margin indicates there are no tumor cells at the margin. That means the cancer is contained in the area nearest to the tumor.
A close margin means that the space between the cancerous tissue and surrounding normal tissue is less than about 3 millimeters (0.118 inch).
If you have a biopsy resulting in a cancer diagnosis, the pathology report will help you and your doctor talk about the next steps. You will likely be referred to a breast cancer specialist, and you may need more scans, lab tests, or surgery. Your medical team uses the pathology report and the results of the other tests to determine the stage of cancer and to design the best treatment plan for you.
There are several factors that help a doctor decide which type of biopsy to recommend. These include the appearance, size, and location of the suspicious area on the breast. Before discussing biopsy results, let’s first distinguish between the three types of biopsies.
What is fine-needle aspiration?
In most cases, a fine needle aspiration is chosen when the lump is likely to be filled with fluid. If the lump is easily accessible or if the doctor suspects that it may be a fluid-filled cystic lump, the doctor may choose to conduct a fine-needle aspiration (FNA). During this procedure, the lump should collapse once the fluid inside has been drawn and discarded. Sometimes, an ultrasound is used to help your doctor guide the needle to the exact site, whereby sound waves create a picture of the inside of the breast.
If the lump persists, the surgeon or radiologist, a doctor who specializes in medical imaging such as x-rays and mammograms, will perform a fine needle aspiration biopsy (FNABx), a similar procedure using the needle to obtain cells from the lump for examination.
What is a core-needle biopsy?
Core needle biopsy is the procedure to remove a small amount of suspicious tissue from the breast with a larger “core” (meaning “hollow”) needle. It is usually performed while the patient is under local anesthesia, meaning the breast is numbed. During the procedure, the doctor may insert a very small marker inside the breast to mark the location of the biopsy. If surgery is later required, the marker makes it easier for the surgeon to locate the abnormal area. Even if no further treatment such as surgery is needed, the marker allows a breast imaging radiologist to see on future mammograms where the biopsy was done.
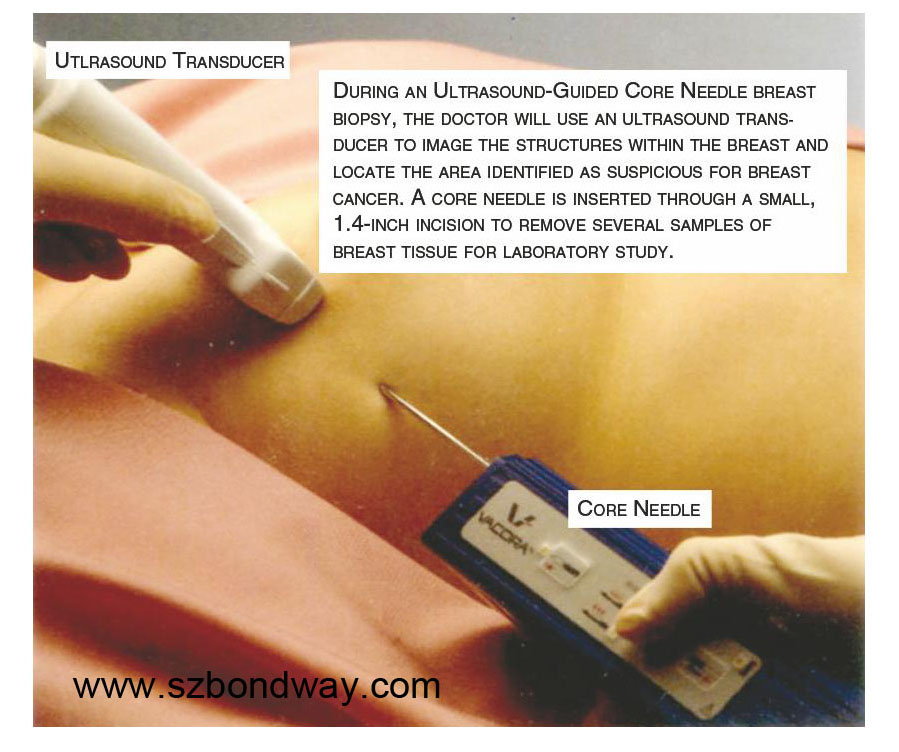
The radiologist or surgeon performing the core-needle biopsy may use specialized imaging equipment to guide the needle to the desired site. As with fine-needle aspiration, this may involve ultrasound.
During an ultrasound-guided core needle biopsy, the patient lies down while the doctor holds the ultrasound against the breast to direct the needle. On the other hand, during a stereotactic-guided core-needle biopsy, the doctor uses x-ray equipment and a computer to guide the needle. Typically, the patient is positioned lying on the stomach on a special table that has an opening for the breast, and the breast is compressed, similar to a mammogram.
Occasionally, no imaging equipment is used, but this is typically only in cases where the lump can be felt through the skin. This type of procedure is called a freehand core-needle biopsy.
There are fewer side effects associated with a core-needle biopsy than with surgical biopsy.
What should I expect from a surgical biopsy?
(Also known as “wide local excision,” “wide local surgical biopsy,” “open biopsy,” or “lumpectomy”)
As with a core-needle biopsy, a surgical biopsy is done while the patient is under local anesthesia. Typically, this test is performed in a hospital setting where an IV and medications are administered to make the patient drowsy.
The surgeon makes a one- to two-inch cut on the breast and then removes all or part of the abnormal lump and often a small amount of normal-looking tissue, known as the “margin.” If the lump cannot be easily felt but can be seen on a mammogram or ultrasound, a radiologist may insert a thin wire to mark the suspicious spot prior to the surgeon performing the biopsy. Once again, a marker is usually placed internally at the biopsy site at the conclusion of the procedure.
What Can Be Learned From The Biopsy Results?
Once the biopsy is complete, a specially trained doctor called a pathologist examines the tissue or fluid samples under a microscope, looking for abnormal or cancerous cells. The pathology report, which can take one or two weeks to complete, is sent to the patient’s doctor. It indicates whether the suspicious area is cancerous and provides a full picture of your situation. For the patient, waiting for results can be a real challenge, but being able to make an informed decision regarding your treatment is well worth it. Your doctor will go over the report with you and, if necessary, discuss the treatment options.
If no cancer cells are found, the report will indicate that the cells in the lump are benign, meaning non-cancerous. However, some type of follow-up or treatment may still be needed, as recommended by the healthcare professional.
If cancer cells are found, the report will provide more information to help determine the next steps.
The report for a core-needle biopsy sample will include tumor type and the tumor’s growth rate or grade. If cancer is found, the pathologist will also perform lab tests to look at cells for estrogen or progesterone receptors.
In the case of a surgical biopsy, the results reveal data about the type, grade, and receptor status of the tumor, as well as the distance between the surrounding normal tissue and the excised tumor. The margin, as we mentioned earlier, shows whether the site is clear of cancer cells.
A positive margin means cancer cells are present at the margin of the tumor. In cases of positive margins, the cancer has spread beyond the immediate area.
A negative margin or clear margin indicates there are no tumor cells at the margin. That means the cancer is contained in the area nearest to the tumor.
A close margin means that the space between the cancerous tissue and surrounding normal tissue is less than about 3 millimeters (0.118 inch).
If you have a biopsy resulting in a cancer diagnosis, the pathology report will help you and your doctor talk about the next steps. You will likely be referred to a breast cancer specialist, and you may need more scans, lab tests, or surgery. Your medical team uses the pathology report and the results of the other tests to determine the stage of cancer and to design the best treatment plan for you.

We’re proud that more and more hospitals and clinical centers at home and abroad are using our reusable biopsy needle brackets during their routine work. If you fail to find the biopsy needle guide for your ultrasound probes on our website, please do not hesitate to contact our sales staff, and we will upload newly developed products onto our official website periodically.
Shenzhen Bondway Electronics Co.Ltd
2019-9-30
 English
English
 中文
中文 Français
Français
 Español
Español Pусский
Pусский








