Preventive & Treatment Measures After Prostate Biopsy (reusable biopsy needle guide)
Preventive & Treatment Measures After Prostate BiopsyUltrasound-guided transrectal biopsy is more common than transperineal routes
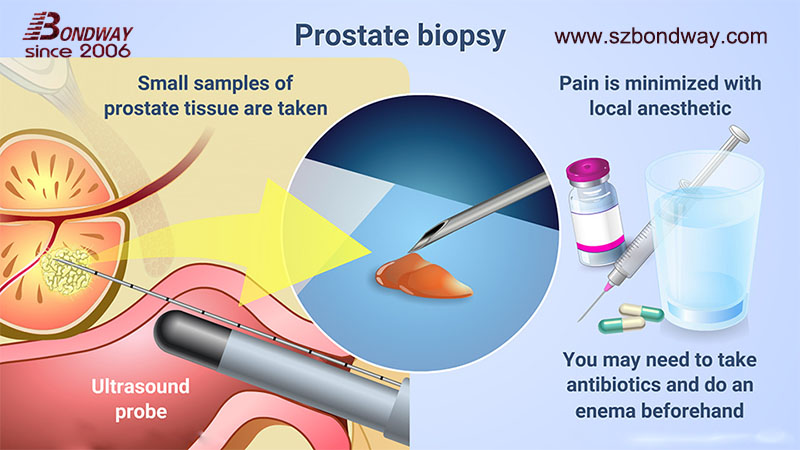
Prostate Cancer (PCa) is one of the most common malignant tumors of urinary system in China. Ultrasound-guided biopsy of prostate tissue is commonly used in clinical histological analysis to clarify the pathological diagnosis, grade and aggressiveness of prostate cancer. According to the path of puncture, prostate biopsy is usually divided into ultrasound-guided transrectal and transperineal routes, of which transrectal prostate biopsy is the most commonly used route.
Infection rate after transrectal prostate biopsy higher
During transrectal prostate biopsy, the needle punctures the rectal mucosa and enters the prostate tissue under the guidance of the ultrasound transducer. During this process, bacteria in the rectum will inevitably be introduced into the prostate tissue and urethra, thus causing infection after the puncture. Therefore, in PCa diagnosis and treatment guidelines of various countries, it is generally recommended to give prophylactic antibiotics before puncture to reduce the occurrence of post-biopsy infection. However, in recent years, due to the abuse of antibiotics and the emergence of drug-resistant bacteria, the infection rate after transrectal prostate biopsy is generally higher than before.
1.jpg)
Reusable biopsy needle guide mounted onto Esaote transducer TRT33
- Prepare for the prostate biopsy
-
- Antibiotic Use
1.1.1 Traditional antibiotics
The PCa diagnosis and treatment guidelines in various countries do not give specific ways and methods on how to use antibiotics to prevent post-puncture infection. Since fluoroquinolones have a broad spectrum inhibition effect on bacteria that may cause post-puncture infection, and can maintain a high concentration in prostate tissue, therefore, In the past, urologists often used fluoroquinolone antibiotics before puncture to prevent post-puncture infection [4]. In recent years, there have been many reports about the increase in infection rate after transrectal prostate biopsy [5-7], among which it has been pointed out that post-puncture infection is mostly caused by bacterial resistance to fluoroquinolones, so whether to continue to use fluoroquinolones to prevent post-puncture infection clinically is worth discussing.
1.1.2 Targeted (sensitive) antibiotics
As noted above, due to the emergence of quinolone-resistant bacteria, empiric or fluoroquinolone antibiotic use is no longer appropriate for every patient. Therefore, some scholars suggest that rectal swab culture before puncture and targeted antibiotics given according to the culture results can effectively reduce the occurrence of post-puncture infection. In 2016, CUSSAN et al. analyzed postoperative infection of more than 4 500 patients with rectal prostate puncture and found that the incidence of infection was only 0.72% in patients given targeted antibiotics before surgery, while 4.55% in patients given empirical antibiotics, indicating that targeted antibiotics can better reduce the occurrence of post-puncture infection. However, due to the fact that rectal swab culture needs to be performed 24-48 h before the puncture, and the operation is complicated and the positive rate of culture is low, it is difficult to widely carry out in clinical practice. Therefore, we believe that targeted antibiotic prophylaxis should only be given to patients with a history of fluoroquinolone resistance and high risk factors for post-puncture infection. In our clinical practice, prophylactic oral moxifloxacin 3 days is usually chosen.
1.2 Rectal Preparation
Some scholars believe that cleaning the rectum before the puncture can effectively reduce the risk of the puncture needle introducing bacteria into the genitourinary system, thus reducing the occurrence of infection. At present, rectal decontamination can be roughly divided into two measures: rectal disinfection and cleaning enema. In general, rectal decontamination before puncture can effectively reduce the incidence of infection after transrectal prostatectomy, and it is simple and easy to perform. Therefore, the authors suggest that routine rectal decontamination is recommended for patients undergoing transrectal prostate biopsy to reduce the risk of postoperative infection.
 (transrectal)1.jpg)
Reusable needle guide mounted onto GE endocavity transducer E8C
1.3 Transperineal prostate biopsy introduced instead
Because the needle does not pass through the rectum, it does not introduce bacteria from the rectum into the prostate tissue and the genitourinary system, the incidence of infection after perineal prostatectomy is theoretically lower.

UA1232 reusable biopsy needle guide attached onto BK ultrasound transducer 8848
2 Preventive measures during prostate biopsy
2.1 Specifications of biopsy needles and number of biopsy needles
As the number of puncture needles increases, the theoretical probability that the puncture needle will introduce rectal bacteria into the genitourinary system will also increase. A recent study proved that the number of needles is proportional to the risk of infection, and the study showed that the risk of infection complications increased when the number of needles was 6, 12, and 18 . However, the study did not investigate the number of serious infections, such as sepsis, or measure infection severity. However, recent studies have also shown that the increase in the number of puncture needles does not increase the incidence of post-puncture infection.
2.2 Disposable biopsy needle used instead
Studies have shown that the use of disposable biopsy needles can effectively reduce the incidence of post-puncture infection. TUNCEL etc compared postoperative infection with disposable biopsy needle and repeatable sterilized biopsy needle, and found that the use of disposable biopsy needle can significantly reduce the occurrence of fever and urinary tract infection after biopsy. However, GURBUZ found that the use of one-time biopsy needles did not reduce the incidence of post-puncture infection. The two studies used similar antibiotic prophylaxis and disinfection measures, and the differences in the final results may be due to differences in technique or needle size used. Therefore, more research is needed to explore whether the use of disposable biopsy needles can effectively reduce the incidence of post-puncture infections.
2.3 How many times of biopsy conducted?
Clinically, for prostate cancer patients with suspected negative initial puncture, close monitoring is usually adopted. If suspicious nodules are found in rectal examination or imaging, prostate specific antigen, When repeated puncture indications such as increased PSA and atypical hyperplasia or multiple high-grade prostatic intraepithelial neoplasia (PIN) at the initial puncture, repeated puncture or even multiple puncture is required. So increasing the number of piercings, will there be an increase in the incidence of infection after the piercing. A study has shown that repeated puncture has no increased risk of infection complications compared with initial puncture. However, the study of EHDAIE showed that the incidence of infection was 2% for patients who received only one or two transrectal prostate punctures, while the incidence of infection was 15% for patients who received five or more punctures. At the same time, relevant studies have also pointed out that the incidence of prostatitis after repeated puncture is much higher than that of patients with initial puncture (6.8% vs. 1.3%). In conclusion, an increase in the number of piercings may increase the occurrence of post-puncture infections.
3 Summary
At present, the incidence of infection after transrectal prostate biopsy is increasing day by day. Due to the emergence of fluoroquinolone-resistant bacteria, the administration of fluoroquinolone antibiotics before puncture can no longer effectively reduce the incidence of infection. At present, effective strategies to reduce infection include the use of targeted (sensitive) antibiotics, pre-puncture enema and rectal disinfection, sterilization of puncture needles during puncture, and strict control of puncture indications to reduce unnecessary puncture. Choosing a reasonable number of puncture needles, using disposable puncture needles and transperineal prostatic puncture can reduce the incidence of post-puncture infection.
.jpg)
Reusable biopsy needle guide mounted onto Terason transducer 8BP4
Statement: This article is reprinted, the purpose is only for fellow friends to learn to improve the level of use. Readers may use the content of the text for study, research or appreciation, as well as other non-commercial and non-profit purposes, but at the same time, please comply with the copyright law and other relevant laws, and shall not infringe on the rights of the original author. If the original author does not agree to publish the content of this article, please contact us to delete it immediately
 English
English
 中文
中文 Français
Français
 Español
Español Pусский
Pусский








